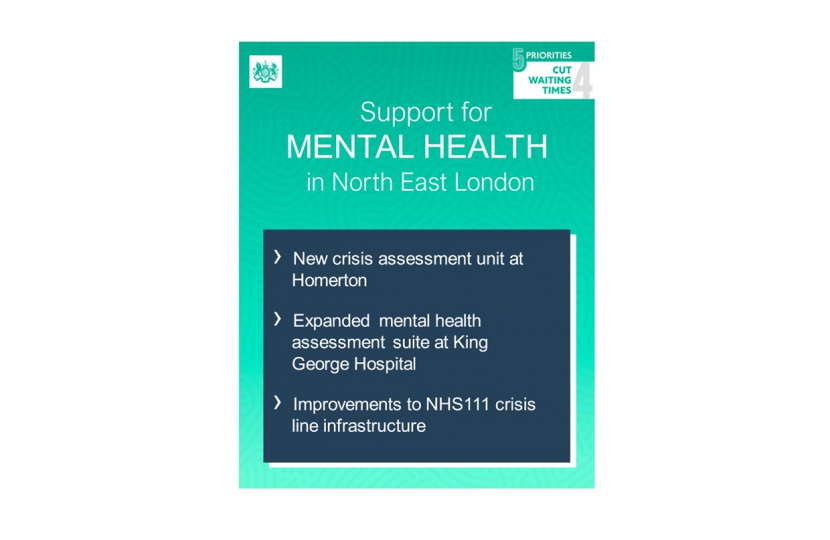
£150m is being invested in NHS mental health urgent and emergency care services until April 2025. The vast majority of this funding will be used to provide new and improved mental health crisis response infrastructure, such as community hubs, step-down facilities and emergency department spaces and is supporting the following local investments in the North East London area:
- £1.57m to expand the mental health assessment suite at King George Hospital
- £286,800 to support improvements to the NHS111/Crisis line infrastructure
- £311,000 to provide a new crisis assessment unit at Homerton Hospital
£7m will support the provision of 100 specialised mental health ambulances to bring staff directly to patients in need of emergency support.
The Health Secretary, Steve Barclay, has also announced an expansion of service to help keep vulnerable people out of hospital. Community services including falls and frailty teams will be scaled up, with up to 50,000 people a month supported by clinicians at home in high-tech ‘virtual wards’. Urgent community response teams will be scaled up to provide more patients with support at home within 2 hours, in recognition of the pressures facing A&E. The government and NHS England have published an urgent and emergency care plan to reduce waiting times and improve care for patients. More information can be viewed here - NHS to expand services to keep vulnerable out of hospital - GOV.UK (www.gov.uk)
Alongside these investments, the Government has announced the priorities for the first year of the Women’s Health Strategy for England which was first published last year. Priorities for the first year include:
- Encourage the expansion of women’s health hubs
- The development of a pregnancy loss certificate to aid women who experience a loss before 24 weeks of pregnancy
- Improved access to fertility treatments
- Improved access to hormone replacement therapy (HRT)
- Improving information provision on women’s health, especially for girls in schools
Julia Lopez MP said: ‘The impact of timely mental health support, particularly for those undergoing a moment of crisis, has been clear from my discussions with senior health leaders in the community and from families who have called upon them. The expansion of the mental health assessment suite at King George Hospital will have an immediate impact and will help to reduce pressures upon other services. I look forward to receiving further updates on the progress of these works from NELFT.
I also welcome the gathering momentum on our Women’s Health Strategy as we enter it’s first year of operation. Last year a number of women contacted me to highlight their struggles in accessing HRT medicines and the introduction of a pre-payment certificate in April of this year will greatly assist in this.’

